Cardiovascular Disease (CVD) is the number one killer for Australians, yet most of these deaths are preventable. Cardiovascular disease accounts for 27% of deaths in Australia. Around 1.2 million Australians have 1 or more heart or vascular conditions. CVD is an umbrella term for conditions that effect the heart and blood vessels.
Atherosclerosis is the main contributor to CVD. It is characterised by a chronic inflammatory response within tissues resulting in plaque forming on the intima layer of the arteries. Consequently, resulting in thicker vessel walls and a reduced lumen area. This is an underlying contributor to CVD because less blood can flow through the vessels and more strain is put on the heart.
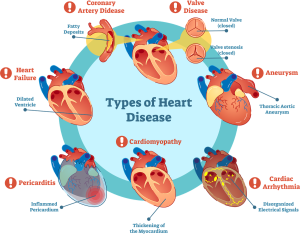
The most common forms of CVD are;
Heart attack –Acute myocardial infarction, also known as a heart attack, is a life-threatening condition that occurs when blood flow to the heart muscle is abruptly cut off, causing tissue damage. This is usually the result of occlusion in one or more of the coronary arteries. A blockage can develop due to a build-up of plaque, a substance mostly made of fat, cholesterol, and cellular waste products or due to a sudden blood clot that forms on the blockage.
Stroke – The most common type of stroke is ischemic stroke. This happens when plaque or a blood clot blocks blood flow to an artery in or on the brain. Haemorrhagic stroke is less common. This happens when a blood vessel breaks open and leaks blood into the brain. A transient ischemic attack (TIA) is similar to an ischemic stroke, but the blood clot breaks up after a short time, usually before there is long-term damage.
High blood pressure> – Consistently high BP in arteries that increases the development of atherosclerotic plaque due to the increases demand on lumen walls. Hypertension = 140/90, risk factor for cardiovascular disease due to the increased myocardial demand.
Chronic heart failure: heart is unable to pump blood at a rate that is adequate for the metabolising tissue. Low stroke volume = low ejection fracture and consequently less oxygen getting to the muscles. Guidelines for the prevention, detection and management of chronic heart failure in Australia include “Participating in regular physical activity” as the number one priority for management and prevention.
Atrial Fibrillation: disorganised atrial electrical activity – rapid and irregular ventricular depolarisations. Often associated with heart failure.
Risk factors – non-modifiable and modifiable
There are risk factors that can’t be changed (sex, age, and family history), but most risk factors of CVD are modifiable. These include high cholesterol (>5.5mmol/L), obesity (<24.9 BMI), smoking, high blood pressure, alcohol use (over 2 standard drinks p/d), sedentary lifestyle (>150m p/w), stress and depression.
Exercise Benefits
Exercise has a favourable effect on many of the established risk factors of CVD, such as weight reduction, cholesterol reduction, increase mental health and decrease blood pressure.
Exercise Sports Science Australia (ESSA) the governing body of Exercise Physiology says that people need 150 minutes of moderate activity per week to decrease blood pressure and maintain healthy cardiac function.
Exercise benefits for cardiac and circulation – exercise increases stroke volume, increases diastolic, decreases Hr, increase myocardial perfusion (more oxygen for the muscles), lower resting levels of catecholamine, potential increases in ejection fraction, increased peripheral vasodilation. In layman’s terms – it improved exercise tolerance, vo2 peak and peripheral blood flow.
Exercise benefits for skeletal muscle – increase mitochondrial number and density, increases capillary, increases muscle fibre size and bulk, increases type 1 muscle fibres, increases oxidative enzymes, and delays anaerobic metabolism. Layman’s terms – Improved oxygen extraction, muscle strength and endurance.
Exercise benefits ventilation and others – reduced shortness of breath and perceived exertion scores, decreased oxygen demands at submaximal workloads, improved quality of life, sleep quality, mental health, and increase/maintain bone density.
Exercise Prescription
Aerobic – 11-13 RPE. Requires supervision and monitoring of HR and BP (but using RPE). 8-10 minute warm-up to reduce adverse cardiovascular effects including ST segment depression, arrhythmias, and transient LV function, increase blood flow & skeletal muscle perfusion, reduce muscle viscosity, and reduce injury risk. 8-10 minute cool down to reduce venous pooling, dizziness and post-exercise hypotension. 5 days per week.
Resistance – requires supervision, avoid Valsalva manoeuvre (as it raises blood pressure), 12-20 reps at low intensity, including 8-10 exercises. Progress intensity and reduce reps to 8-12 after 6-8 weeks of training. Heavy weightlifting of intensive and isometric nature should be avoided as it causes further increase in blood pressure. Often this can be an advertisement as most people with these conditions will be overweight and would like to hear that it would be “easy” to start off with.
Bottom line is to get exercising!!
We have a range of options here at The Body Refinery, talk to our friendly front desk.