The number of cancer survivors worldwide is growing each year. Cancer survivors face unique challenges and changes to their health as a result of the cancer itself as well as side effects from treatment. Cancer survivors often experience declines in quality of life and physical functioning as well as an increased risk of cancer recurrence. In 2009, Exercise & Sports Science Australia published the first-ever position statement on exercise guidelines in the world for people with cancer. Since then, there has been exponential growth in research evaluating the role of exercise during cancer treatment.
What is cancer?
Cancer is a disease of the basic building blocks of the human body, the cells. Cells are constantly regenerating in order to heal injuries, grow and replace. Cancer occurs when this process goes awry, and the cells become abnormal. As this process continues and the cells divide further, a lump forms which is called a tumour. Cancerous tumours spread to nearby tissue and can travel to distant parts of the body where new tumours form. There are more than 100 types of cancer, and they are generally named after the organ or tissue from which it originated.
How is cancer treated?
The combination, or pathway, of treatment a patient chooses depends on the type and stage of cancer. The most common types of treatment are: surgery to remove cancerous cells; chemotherapy using chemicals to attack the cancer; and radiation therapy, where radiation is targeted to reduce or kill a tumour.
How does exercise help?
Research shows that exercise benefits most patients before, during and after cancer treatment. Specifically for cancer patients, exercise may:
- Improve the body’s response to treatment.
- Reduce the risk and severity of side effects of cancer treatment.
- Reduce surgery complications and time spent in the hospital.
- Help maintain a healthy weight.
- Improve recovery from treatment by: increasing energy levels; reducing treatment-related muscle loss; stringing bones and improving mobility and balance.
- Improve sleep
- Reduce fatigue
- relive Relieve stress, anxiety and depression.
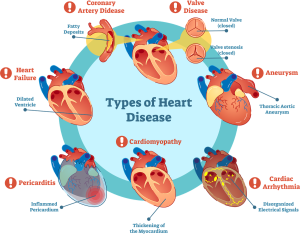
- Reduce the risk of developing high blood pressure, heart disease, stroke, osteoporosis and Type 2 diabetes.
- Reduce the risk of certain cancers returning, including breast, prostate, and bowel cancers.
- Boost mood and self-esteem.
How much exercise is appropriate?
Exercise goals for anyone, including those undergoing or recovering from cancer treatment, should be based on being as physically active as their abilities allow. Exercise for cancer patients will look different for everyone, depending on the type of cancer, stage, and side effects. The Clinical Oncology Society of Australia states that people with cancer who are relatively healthy and have been assessed as low risk, should include 2.5 hours of moderate-intensity aerobic/cardio exercise or 1.5 hours of vigorous aerobic/cardio exercise per week. As well as this, 2-3 strength resistance sessions per week should be undertaken to build muscle strength. If it has been a while since someone has been active, or their fitness level is low, it’s important to begin slowly and build up gradually.
Where to from here?
If you are undergoing treatment for cancer or recovering from cancer and would like more information or an exercise program that is tailored to your personal needs and circumstances, speak to an accredited Exercise Physiologist about how much and what type of exercise is best for you.
We are lucky to have very qualified and talented Exercise Physiologists here at The Body Refinery, in New Farm. Book your appointment today.
Article written by Jess Crawford, Exercise Physiologist.